Periodontal disease, also called gum disease, is a chronic inflammatory disorder of the gums and the supporting bone structure of the teeth. The accumulation of bacterial plaque is primarily responsible for the development of gum disease. It is not an irritation, but a progressive infection that destroys the attachment fibers and alveolar bone, leading to tooth loss if left untreated.
The genesis of the pathology is the colonization of the tooth surface by bacteria, which initiates an immunoinflammatory response. The response is typically aimed at protecting the body, resulting in the breakdown of the periodontium. Periodontal disease is not always symptomatic in the early stages of its development. Thus, the extent of the underlying destruction remains hidden until one realizes that considerable damage has been done.
This blog explains the signs of periodontal disease, from the hidden signs of initial gingivitis to the severe symptoms of advanced periodontitis. Once you learn to recognize these key indicators, you will know when to seek your dentist's intervention to prevent the disease from further developing and maintain your oral health in the long term.
The Early Warning Signs and Symptoms of Gingivitis Stage
Periodontal disease rarely begins with tooth loss. The disease often starts with a subtle, silent stage called gingivitis. It is the stage of gum disease that can be completely reversed, but it is also the most common stage that patients tend to neglect. You may think that your mouth is healthy since you are not experiencing pain, but the absence of pain does not necessarily mean that it is not infected. During this initial stage, the bacteria in the dental plaque attach along the gumline, releasing toxins that irritate the soft tissue. If you do not eliminate this plaque through brushing and flossing, the body initiates an inflammatory reaction.
The early warning signs include:
Bleeding Gums While Brushing or Flossing
One of the most pervasive myths in oral health is the idea that gums bleed because they are being cleaned too vigorously. Healthy gum tissue is strong, and it does not bleed when subjected to the normal force of brushing or flossing. Should you find that when you spit in the sink, a pinkish tint appears in the saliva, or you find that when you use your dental floss, you see blood, it is a direct indication of active infection.
The reason behind this bleeding is that the epithelial lining of the gum pocket, the small crevice between your tooth and gum, has been ulcerated by the presence of bacterial toxins. When you tear this already inflamed tissue with a toothbrush or floss, the micro-ulcerations open, allowing blood to flow.
There is a link between smoking and bleeding of gums, which you should know. Nicotine acts as a vasoconstrictor, meaning it causes the blood vessels to constrict and decrease blood flow to the peripheral tissues, including the gums. A smoker may have gum disease, yet no bleeding whatsoever, because the blood vessels in the smoker are chemically closed. This absence of bloodshed can give you a false sense of security, masking the destruction happening beneath the surface.
For non-smokers, however, bleeding is the primary indicator of gingivitis. It is how the body attracts immune cells to the site of infection. Without paying attention to this indicator, the plaque hardens into tartar or calculus, which further irritates the gum tissue and accelerates the disease process. You need to take bleeding gums just as seriously as you take a bleeding wound on your hand; it needs to be attended to, diagnosed, and treated.
Redness, Swelling, and Tenderness
Normal and healthy gum is usually coral-pink in color, firm, and can be stippled, which resembles the skin on an orange. When gingivitis ensues, the appearance will not be the same because the inflammatory response, known as edema, will cause a similar appearance. The blood vessels swell to deliver blood to the infected region in an attempt to kill the bacteria, and the gums fill with fluid, becoming engorged.
Therefore, the tissue changes to a darker, furious red or even violet, instead of a healthy pink. The texture also varies as it is no longer hard and stippled but puffy, soft, and shiny. It forms a deeper pseudopocket around the tooth, providing more room where bacteria can build up in areas that your toothbrush is unable to reach.
You can also experience soreness in the gums or when you are eating some food. This sensitivity is a direct consequence of the accumulation of pressure in the tissue resulting from inflammation. Although this pain is not severe in the initial phases, it is a clear indication that the biological balance of your mouth has been broken. This redness and swelling are usually localized at the spots where the plaque has been left undisturbed.
You may observe that you have puffy and reddened gums around your back teeth, and the front teeth seem healthy. This localization indicates where exactly your oral hygiene is falling short. However, when the redness is extensive, it is an indication of a more generalized infection or a systemic problem with your immune system. You can detect them early enough before they lead to a lot of pain by visually examining your gums using a bright mirror.
Persistent Bad Breath or Halitosis
After a heavy meal with garlic or onions, or when we wake up in the morning, we all have bad breath, which is a temporary effect. However, chronic bad breath, the medical term for which is halitosis, persists despite brushing, flossing, or mouthwash use, and is a clear clinical indicator of periodontal infection.
The food you have eaten does not produce this odor, but it is the metabolic byproducts of the bacteria in your mouth. The gum disease-causing bacteria are mainly anaerobic, meaning they thrive in the absence of oxygen, such as deep within the gum pockets. These bacteria break down proteins and food debris, releasing Volatile Sulfur Compounds (VSCs), which have odors of rotten eggs or rotting organic materials.
The growth of these bacteria is exponential in nature when you have gum disease, resulting in a continuous generation of these vile gases. You may also experience a lingering bad taste in your mouth, which is typically described as metallic or sour. This taste is the sense experience of the purulent secretions and bacterial excrements oozing out of the infected gum crevices.
There is no point in trying to cover up the odor with breath mints or cosmetic mouth rinses, since the cause of the odor is deep below the gumline and cannot be reached by these products. It is essential to note that if you continue to feel self-conscious about your breath, or whenever someone you love mentions it, you should consider the high likelihood that periodontal disease is the culprit. This sign indicates that the bacterial count in your mouth is so high that your body can no longer tolerate it, and you require a professional cleaning to eliminate the cause of the infection.
Advanced Symptoms Signalling Periodontitis Stage
Unless the initial symptoms of gingivitis are recognized and treated, the disease can progress to periodontitis. The infection penetrates the superficial soft tissues into the deeper structures that hold the teeth, such as the periodontal ligament and the alveolar bone. At this point, it is too late to take action. The lost bone will not regenerate itself. Your periodontitis symptoms are worsening, which means your dentition is weaker in its structure. It is essential to recognize these high-tech red flags, as they are the last warning signs of tooth loss being an inevitable outcome.
Gum Recession
The term "long in the tooth" is used to refer to aging; however, in dentistry, it is a pathological effect of gum disease rather than an ordinary result of aging. The reason is that gum recession is a condition in which the margin of the gum tissue surrounding the teeth is worn away or pulled back, exposing more of the tooth or the root of the tooth.
This is because the inflammation that develops into chronic degeneration of the underlying bone and the gum tissue moves in the direction of the bone level. The teeth then seem to be longer than they were when your gums were receding. It is not a visual illusion; you do see some of the tooth that is meant to be covered by the gum and bone.
Exposed tooth root is an aesthetic issue and poses significant functional problems. The cementum that covers the root in the case of the tooth is far softer and more porous than the hard, protective enamel that covers the crown of the tooth. Once this delicate root structure is exposed to the oral environment, you may experience sharp and sudden pains when consuming hot, cold, or sweet foods and drinks.
This hypersensitivity of the dentin is because the microscopic tubules in the root conduct the stimulation straight to the tooth nerve. Moreover, the root surface is very vulnerable to decay. Root caries (holes on the root) develop at a high rate and may destroy a tooth far quicker than a cavity on the crown. In case you realize your smile is different, or you feel there is a notch along the gumline with your fingernail, you are probably experiencing gum recession caused by periodontal loss of attachment.
Deep Pockets and Pus
The distance between the tooth and the gum (sulcus) is generally between one and three millimeters in a healthy mouth. This is a shallow depth that enables you to clean the area well with the help of a toothbrush and floss. As periodontal disease progresses, however, the attachment fibers between the gum and the tooth are destroyed, and this space deepens to create a periodontal pocket. Your pocket cleaner can never clean a pocket more than four millimeters in depth; your toothbrush simply cannot reach the bottom of it. The pockets develop as bacterial reservoirs, food debris, and tartar, which form a vicious circle of infection and destruction.
The presence of pus, or suppuration, is one of the most terrifying symptoms of such deep pockets. Pus is a thick, yellowish-white liquid that is made of dead white blood cells, tissue debris, and bacteria. It is the physical evidence that cannot be refuted, indicating that your body is struggling with a severe, active infection. When you bite down, you may feel pus coming out of the gums, or when you press on a specific part, you may taste it. It is practically an abscess that empties into your mouth.
The presence of pus indicates that the infection is severe enough to cause tissue necrosis. It is not an issue that home remedies will solve. It needs professional periodontal therapy to debride the infection, clean the root surfaces, and decrease the pocket depths to a sustainable size. It is risky to neglect the presence of pus, as the bacteria of this infection may spread to your bloodstream and affect other parts of your body, which can also lead to problems such as cardiovascular disease and difficulties in managing diabetes.
Loose or Shifting Teeth
After a heavy meal with garlic or onions, or when we wake up in the morning, we all have bad breath, which is a temporary effect. However, chronic bad breath, the medical term for which is halitosis, which does not go away despite brushing, flossing, or mouthwash, is a clear clinical indicator of periodontal infection.
The food you have eaten does not produce this odor, but it is the metabolic byproducts of the bacteria in your mouth. The gum disease-causing bacteria are mainly anaerobic, meaning they thrive in the absence of oxygen, such as in the deep pockets of the gums. These bacteria break down proteins and food debris, releasing Volatile Sulfur Compounds (VSCs), which have odors of rotten eggs or rotting organic materials.
The growth of these bacteria is exponential in nature when you have gum disease, resulting in a continuous generation of these vile gases. You may also experience a lingering bad taste in your mouth, which is typically described as metallic or sour. This taste is the sense experience of the purulent secretions and bacterial excrements oozing out of the infected gum crevices. There is no point in trying to cover up the odor with breath mints or cosmetic mouth rinses, since the cause of the odor is deep below the gumline and cannot be reached by these products.
If you continue to feel self-conscious about your breath, or whenever someone you love mentions it, then you should consider the high likelihood that periodontal disease is the culprit. This sign indicates that the bacterial count in your mouth is so high that your body can no longer tolerate it, and you require a professional cleaning to eliminate the cause of the infection.
Why Pain Is the Last Sign to Appear
The greatest misjudgment is to rely on pain as the primary measure of your oral health. Periodontal disease is infamously referred to as a disease with no symptoms since it seldom causes acute pain until an advanced stage of the disease. The nerve supply of the gums is not the same as the nerve supply of the teeth.
It is possible to have enormous destruction of the gum tissue and bone without the sharp, intense, painful sensation of a cavity or a broken tooth. You will be experiencing throbbing pain by the time you realize that you have formed an acute abscess or the infection has spread into the nerve of the tooth itself.
This lack of initial pain is the reason behind the insidious nature of gum disease. It enables patients to rationalize their symptoms, for example, the ignorance of bleeding, bad breath, and recession, as it does not cause pain. Understand that the disease is alive and destructive, irrespective of your level of comfort.
Delaying until the pain comes about before treatment is practically delaying until the tooth is hopeless. The above signs are the real signs of disease activity. These include:
-
Bleeding
-
Swelling
-
Odor
-
Recession
-
Pockets
-
Mobility
These visual and functional indications must be relied upon at the expense of the feeling of pain.
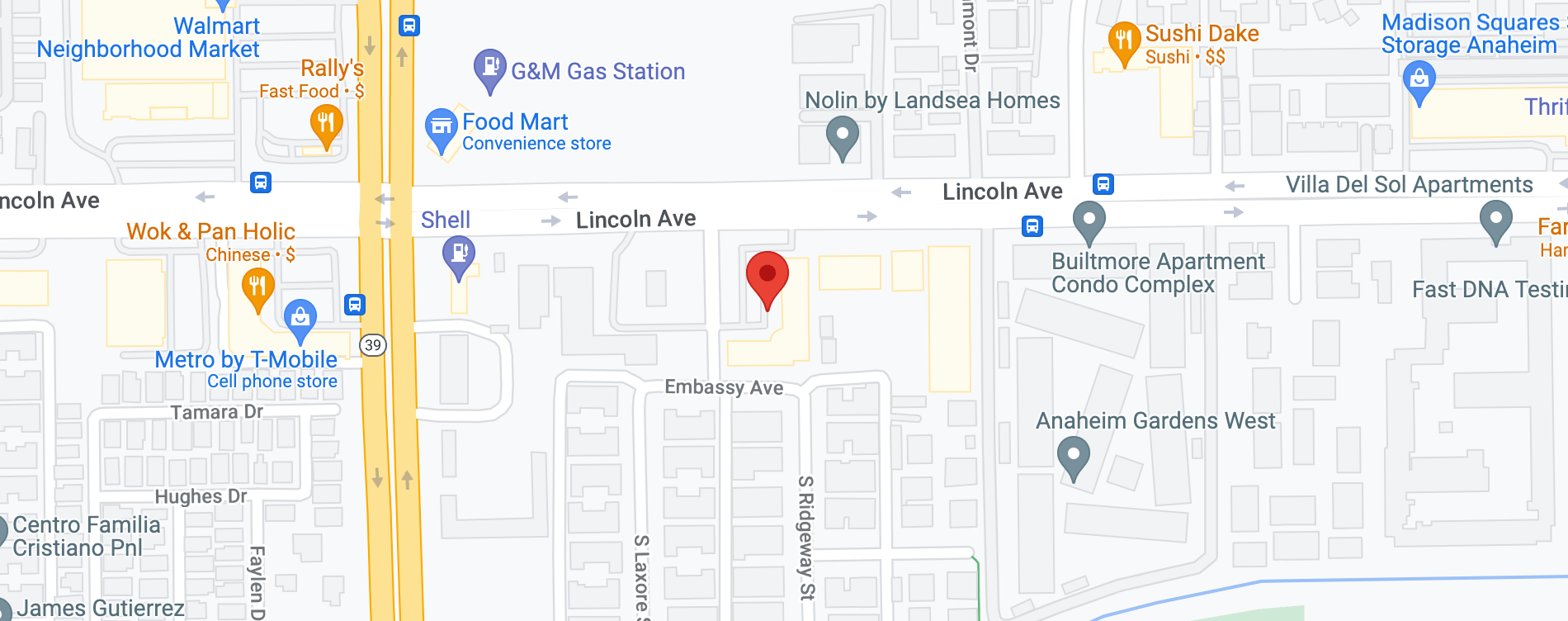
Find an Experienced Dentist Near Me
If you experience gum disease symptoms outlined above, such as bleeding during a hygiene routine or changes in the gum structure, an urgent professional examination is necessary. Periodontal disease is a degenerative condition that is not self-limiting; however, early intervention by a dentist can prevent the disease and restore healthy tissue. You should not wait until the point of pain, as in most cases, it is too late.
At Anaheim dentist, our clinical team utilizes the latest diagnostic tools to accurately assess your condition and develop a personalized treatment plan tailored to your specific dental needs. We will ensure that we protect your periodontal health using evidence-based treatments tailored to your individual dental problem and needs. Call us at 714-995-4000 to schedule an appointment in Anaheim for a comprehensive gum disease assessment and receive a personalized treatment plan.